IN VITRO FERTILIZATION (IVF)
In vitro fertilization, commonly referred to by the acronym IVF, offers an innovative and technological solution to the challenges of infertility faced by couples aspiring to parenthood. The crucial steps of IVF include: Hormone therapy to prepare for egg retrieval, initiation of fertilization in the laboratory, where sperm meets the egg outside the woman's body. Once this phase is successful, the resulting embryo is delicately implanted into the uterus - Embryo Transfer to the prospective mother, in the hope that pregnancy will follow. In vitro fertilization (IVF) is a crucial step for many people struggling with infertility. After undergoing phases of ovarian stimulation and egg retrieval, the embryo transfer moment is highly anticipated. This step marks the beginning of an anxious waiting period, typically 9 to 14 days, before knowing if pregnancy is successful. It is noteworthy that, according to statistics, seven out of ten couples undergoing IVF treatments succeed in becoming parents, and this success does not solely depend on medical treatments.
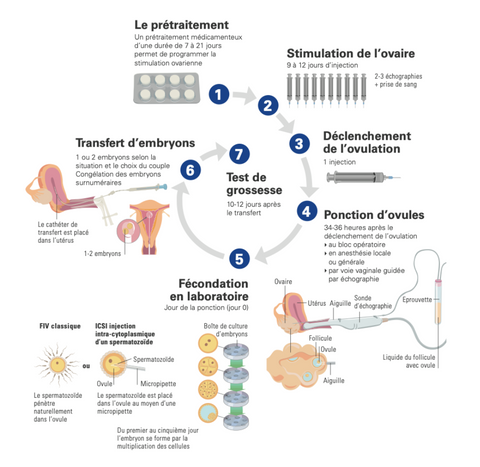
DIFFERENT STAGES OF IVF
Phase 1: Ovarian Stimulation
During this initial phase, the patient undergoes hormonal treatment for approximately 14 days (more or less depending on the dosage but also on each woman's responsiveness). This treatment aims to stimulate the ovaries to promote egg production. It involves the use of a GnRH analogue medication to suppress the patient's natural cycle, control ovulation, and trigger it at the optimal time. Daily injections of follicle-stimulating hormone (FSH or HMG) are also administered to encourage the production and growth of ovarian follicles containing eggs. Regular ultrasound scans are conducted to monitor stimulation.
Phase 2: Triggering
Once the follicles have reached the appropriate size, the patient receives a final injection of a specific hormone triggering ovulation. Egg retrieval is scheduled 36 hours after this injection. (This injection - Ovitrelle - remains in the body for 10 days post-triggering, which unfortunately can skew pregnancy test results).
Phase 3: Egg Retrieval
Egg retrieval, or follicular puncture, takes place under general anesthesia and lasts about twenty minutes. A specialist performs the puncture through the vaginal walls, collecting the eggs by aspirating follicular fluid, all under ultrasound guidance. After the procedure, the patient receives a few hours of rest. It is also important to note that women affected by PCOS (polycystic ovary syndrome) unfortunately have a higher chance of suffering from ovarian hyperstimulation.
Ovarian Hyperstimulation and PCOS - Ovarian stimulation during IVF in women with polycystic ovary syndrome (PCOS) carries certain risks. In the presence of PCOS, the therapeutic margin of FSH (follicle-stimulating hormone) is narrow, making ovarian stimulation more delicate and may lead to ovarian hyperstimulation syndrome (OHSS). Women with PCOS are already more likely to develop OHSS, a potential complication of IVF where the ovaries become swollen and painful due to high levels of hormones used to stimulate egg production. Moreover, egg retrieval during IVF can be more challenging due to ovarian hypertrophy (excessive follicle development), making it more difficult for the doctor to access and retrieve the eggs. It is therefore essential for women with PCOS to consult with a fertility specialist experienced in PCOS treatment to ensure the best possible outcome.
Ovarian hyperstimulation syndrome (OHSS) can manifest with the following symptoms:
- Abdominal bloating
- Nausea with or without vomiting
- Diarrhea
- Feeling of breathlessness
- Rapid weight gain
- Pelvic or abdominal pain
- Vomiting
- Decreased urination
These symptoms can be mild, moderate, or severe. In case of severe symptoms, it is important to immediately consult a healthcare professional for evaluation and appropriate management.
In cases of severe OHSS, hospitalization may be necessary, with specific treatment to manage complications. In the case of overstimulation, it is important to be monitored to prevent worsening and to restore volume with adequate fluid intake.
Source: Heijnen, EMEW, Eijkemans, MJC, Hughes, EG, Laven, JSE, Macklon, N. 3. and Fauser, BCJM (2006). A meta-analysis of conventional IVF outcomes in women with polycystic ovary syndrome. Update on Human Reproduction, 12(1), 13-21.
Xu, Y. and Qiao, J. (2021). Comparison of in vitro maturation and in vitro fertilization in patients with polycystic ovary syndrome: a systematic review and meta-analysis. Annals of translational medicine, 9(15).
Phase 4: Fertilization
Sperm is collected on the same day as egg retrieval, after a period of sexual abstinence of two to four days. It is prepared in the laboratory to fertilize the eggs. These eggs, identified in the follicular fluid, are transferred to a culture medium to be fertilized by sperm (IVF). Fertilization results are observed approximately 20 hours later. The embryos obtained are preserved in culture.
Sixteen days after the egg retrieval, transfer is scheduled 3, 5, or 6 days after fertilization depending on the number of embryos.
Frozen or Fresh Embryo Transfer - What are the Differences?
Embryo transfer can be fresh or frozen (FET), for example, in the case of overstimulation, there will be no fresh transfer. Fresh and frozen embryo transfer have significant differences. Here is an overview of the key differences:
Fresh Embryo Transfer
- Embryos are transferred shortly after fertilization.
- May be associated with a higher risk of ovarian hyperstimulation syndrome (OHSS).
- May be followed by multiple transfer attempts in case of failure.
Frozen Embryo Transfer
- Embryos are frozen and transferred later.
- May offer better success rates, as it allows the uterus to recover from the ovarian stimulation process.
- May reduce the risk of OHSS.
- May be associated with comparable or even better neonatal outcomes compared to fresh embryo transfer.
In summary, the choice between fresh and frozen embryo transfer depends on the specific situation of each person, and it is important to discuss the advantages and disadvantages with a doctor to make the best decision.
Embryo Quality and Developmental Stages:
The development of embryos during IVF occurs in several stages. Here is an overview of the main stages of embryo development:
- Day 0: Fertilization (ICSI)
- Day 1: Fertilization assessment
- Day 2: Cell division - the embryo has between 2 and 4 cells
- Day 3: Cell division - the embryo has between 6-8 cells
- Day 4: Compaction - formation of morula (16-32 cells)
- Day 5: Formation of blastocysts (advanced embryos)
Implantation rates are higher depending on the embryo's development.
The chances of embryo implantation are higher depending on its stage of development. An embryo that has reached the blastocyst stage has the best chances of implantation because it has reached the stage of embryonic competence, meaning it is capable of implanting in the endometrium. Indeed, the implantation rate of blastocysts is better than that of cleavage-stage embryos (Day 5 48% vs. Day 3 32%). Therefore, transferring a blastocyst-stage embryo is often preferred to increase the success rate of IVF.
Source: Glujovsky D, Farquhar C, Quinteiro Retamar AM, Alvarez Sedo CR, Blake D. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database of Systematic Reviews 2016, Issue 6.
Phase 5: Embryo Transfer
Between 3 and 6 days after fertilization, one or two embryos are delicately transferred into the uterus using a fine catheter. After this painless procedure, the patient can resume normal activities. Untransferred embryos can be cryopreserved, offering the possibility of later use during a thaw cycle, with a legal storage duration of 10 years.
FIV Journey Schema
Phase 6: Pregnancy
Monitoring Blood analysis is performed to check for the absence of the beginning of multiple pregnancies. The main complication associated with ART is the possibility of multiple pregnancies, increasing risks for both the mother and the babies. Maternal complications include diabetes, hypertension, preeclampsia, and premature birth. In newborns, the risks of prematurity and malformations are increased. To prevent this, measures are taken, including pregnancy termination. In case of a negative result, further treatments are discussed during a consultation with your doctor.
FACTORS THAT INFLUENCE EMBRYO IMPLANTATION
- Embryo development stage: Blastocyst implantation rates are better than those of cleavage-stage embryos (Day 5 48% vs. Day 3 32%). It is suggested that naturally conceived embryos are generally found in the fallopian tube on Day 3 rather than in the uterus. Therefore, the uterus may not be the optimal environment for embryos at this early stage.
- Patient's age: Implantation chances decrease with age. Ovarian reserve decreases with age, meaning fewer available eggs and reduced egg quality. Additionally, underlying medical conditions associated with age can also affect fertility and the uterine environment.
- Embryo quality: Morphology and viability of the embryo are determining factors.
- Endometrial condition: Endometrial thickness and preparation influence implantation. This includes thickness, texture, and level of blood irrigation. Inadequate endometrium can compromise the embryo's ability to implant and develop.
- Synchronization between embryo and endometrium: Transferring a frozen embryo can circumvent issues related to synchronization between embryo development and endometrial receptivity. For successful implantation, it is crucial for the embryo to be transferred into the uterus at the optimal time when the endometrium is most receptive. In some cases, such as with frozen embryos, this synchronization can be adjusted to increase implantation chances.
- Sperm quality: Sperm quality can also influence implantation chances. Poor sperm quality can affect fertilization and embryo development. Comprehensive sperm analyses are often performed to assess concentration, motility, and morphology (IVF ICSI).
- Number of embryo cells: The number and quality of embryo cells are important indicators. The number and quality of embryo cells can provide indications of the embryo's ability to develop successfully. An embryo with an appropriate number of cells and normal cell division is more likely to implant and continue to develop properly.
Therefore, to prepare for its transfer, one must prepare one's body naturally on several points:
- Oocyte quality
- Endometrium (receptivity, thickness, etc.)
- Inflammation and the immune system
- Husband's sperm
RECOMMENDATIONS FOR THE POST-TRANSFER PERIOD
Advice for the Post-Transfer Period
After embryo transfer, it is essential to follow some advice to maximize the chances of success and facilitate a smooth transition to the next steps of the In Vitro Fertilization (IVF) journey. However, it is understood that most of the work is done beforehand, especially 90 days before the start of the IVF protocol to prepare the body for this important stage: And no, vitamin B9 and Vitamin alone are not enough to boost your chances of success.
It is also important to maintain a normal life and cultivate a positive attitude. Continue your daily activities, including work, and feel free to exercise, avoiding heavy loads and excessive efforts. Adopting a healthy and balanced diet is crucial, excluding caffeine, theine, tobacco, and endocrine disruptors. These choices contribute to creating an environment conducive to embryo implantation.
Intimate Relations after Transfer
Contrary to some beliefs, intimate relations are not contraindicated after embryo transfer. According to studies, they may even be encouraged. Seminal fluid could play a role in modifying the maternal immune system, thus favoring the acceptance of the embryo by the patient's body and its implantation in the uterine cavity. However, it is crucial to maintain protected intercourse during the ovarian stimulation phase to avoid multiple pregnancies.
The Waiting Period: Managing Anxiety
The waiting period between embryo transfer and the blood pregnancy test can be stressful. It is not recommended to take an early urinary pregnancy test, as it may give erroneous results. Avoid focusing too much on bodily signals, such as light bleeding, tender breasts, fatigue, and nausea, as they may be related to IVF treatment rather than pregnancy. Keep in mind the importance of social support from your family and friends to maintain a positive morale during this waiting period.
NUTRITIONAL SUPPORT
Before and During ART
The IVF Pack proves to be a suitable choice at all stages of Assisted Reproductive Technology (ART), whether during the puncture-transfer phase or even in the context of Artificial Insemination (AI). One particularity of this pack is that it can be continued throughout the IVF journey, including during the transfer and puncture period. To optimize results, it is recommended that you and your partner start taking the supplements from the IVF Pack 86 days before the start of IVF. This prior preparation aims to create optimal conditions for conception. The continuity of supplementation throughout the entire period, covering both transfer and puncture, helps maintain adequate nutritional intake.
It is essential to emphasize that supplement intake can be stopped once the pregnancy test is positive. This flexibility allows adapting the IVF Pack according to the results obtained, thus ensuring a personalized approach throughout the ART journey. By investing in this early nutritional
THE IVF Bundle by Imane Harmonie